
Access The State of Remote Patient Monitoring and Chronic Care Management
New research reveals that healthcare C-suites are moving to implement RPM and CCM to improve patient outcomes, increase satisfaction and build practice value. A new survey
A patient experience only made possible by our platform and clinical services. Designed by doctors. Proven by hundreds of successful implementations. That’s MD Revolution.

Practices significantly improve patient outcomes in a matter of weeks – with low upfront investments – and scale to accommodate increasing patient volumes.
Leverage our comprehensive suite of technologies and core clinical services to effectively care for your patient populations.

Patients using the platform
User generated data points
Claims Generated
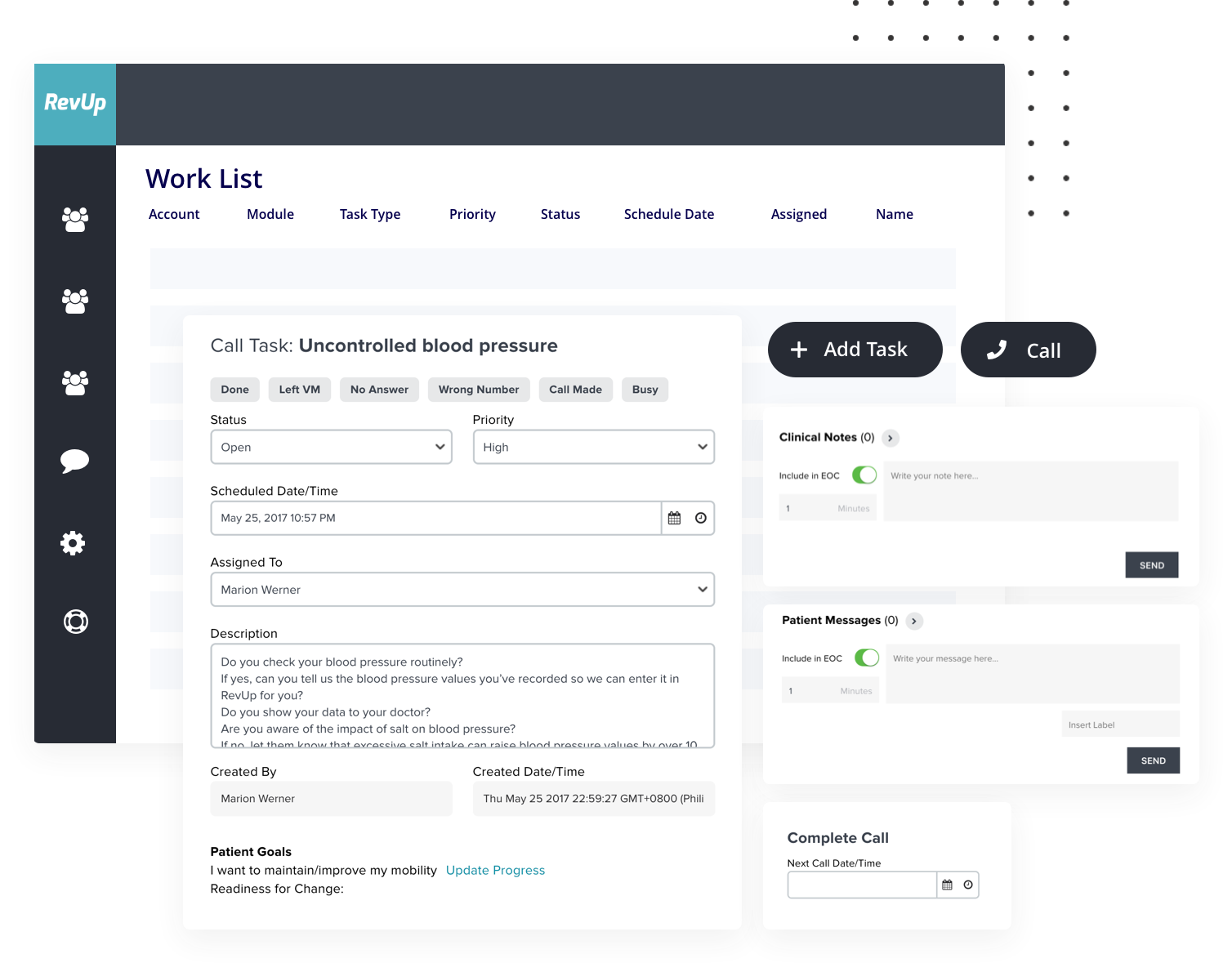
Deliver actionable tasks, outreach and care coordination all working together to achieve more effective patient care, from enrollment through documentation and billing.
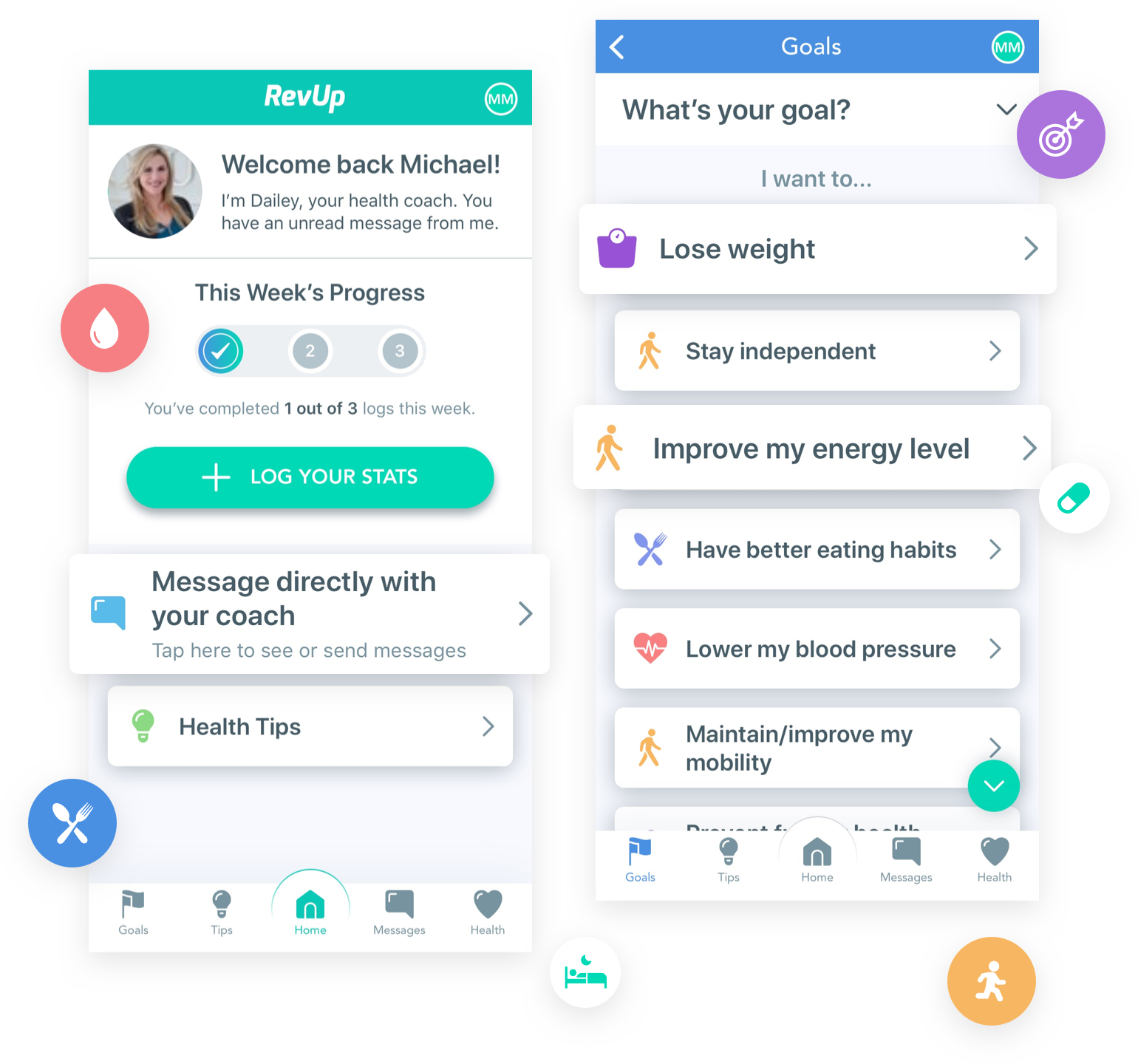
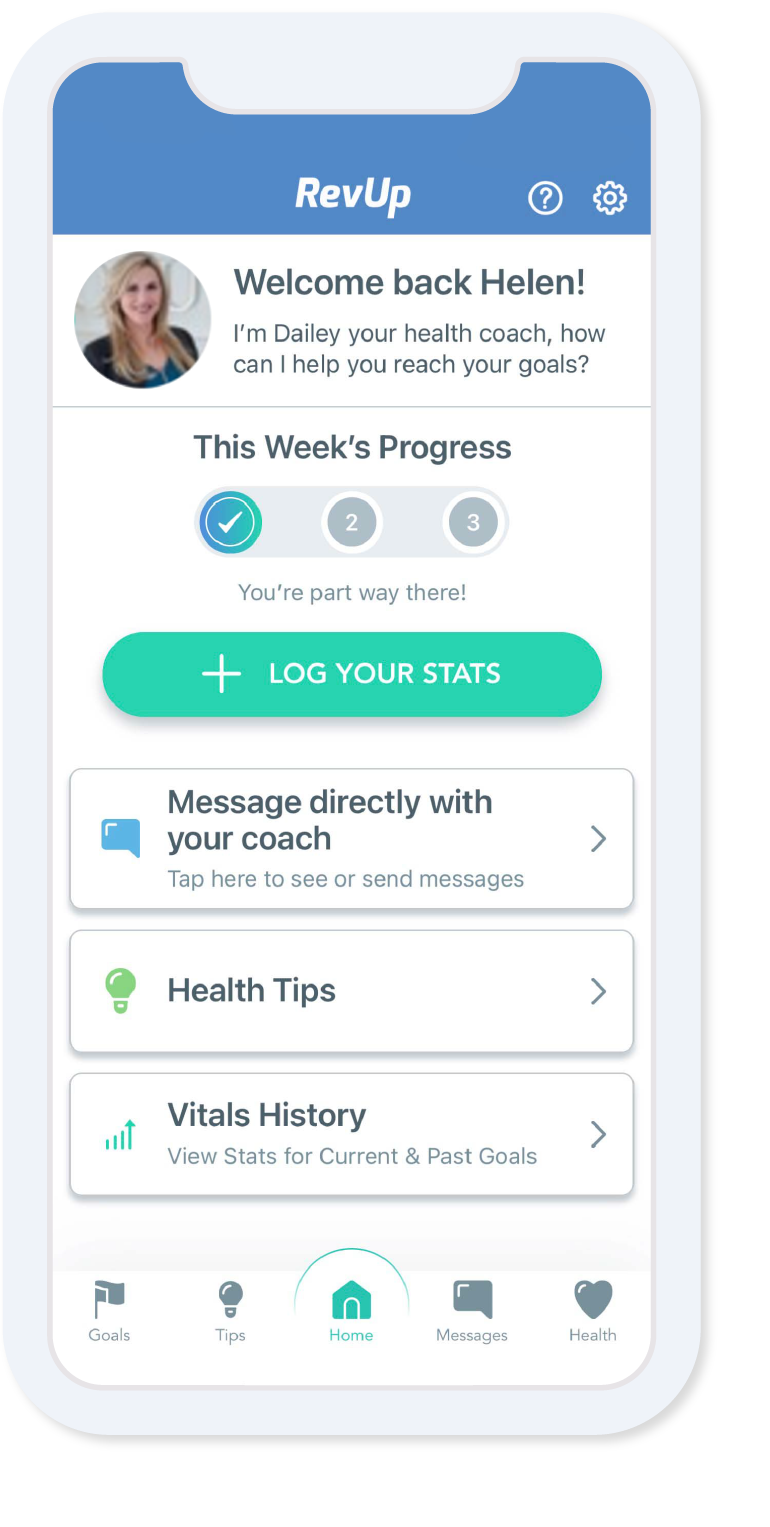
The extensible platform integrates with existing workflows, EHRs, medical devices and health apps so clinical teams and patients can remotely interact with easily navigable tools to sustain engagement via our full-service solutions.
Our time-tested expertise, and the company’s history of hundreds of trusted implementations, successfully guide practices through the patient-centric revolution happening in patient care.

New research reveals that healthcare C-suites are moving to implement RPM and CCM to improve patient outcomes, increase satisfaction and build practice value. A new survey

MD Revolution ranks No. 2,256 on the 2023 Inc. 5000, its annual list of the fastest-growing private companies in America.

San Diego, California, August 1, 2023 — MD Revolution, a leading provider of remote care management and clinical services has acquired NavCare, a remote patient
— Privacy • Terms of Use